
What is Osteoporosis?
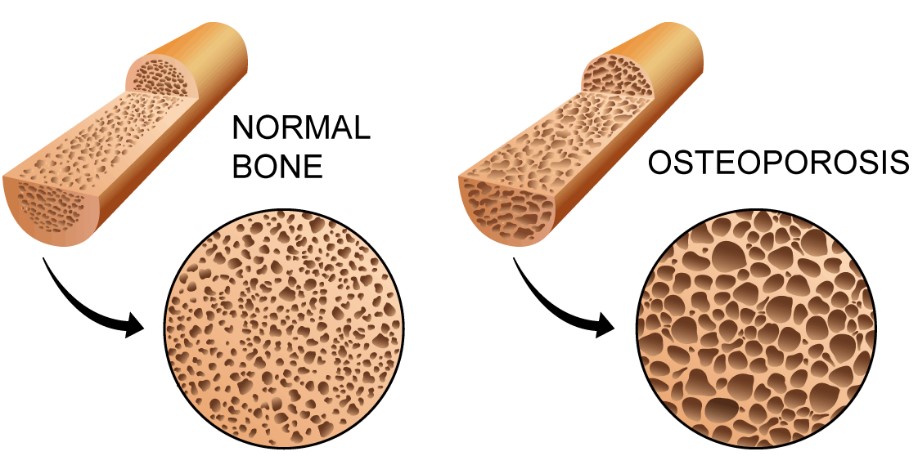
Osteoporosis is a chronic condition that affects our bones, more specifically our Bone Mineral Density (BMD). Osteoporosis is identified using a Dual Energy X-ray Absorptiometry (DXA) Scan to attain a T-Score value for our BMD. This reading indicates how far above/below our BMD is compared to a peak reading of BMD for our gender.
The World Health Organisation classifies that a T-Score value of ≤-2.5 indicates osteoporosis (1). Additionally, those with a T-score between -1.0 and -2.4 are classified as having osteopenia, a slightly less severe case of BMD loss (1). These scans allow us to know exactly where in the body low BMI is located; allowing us to plan treatment appropriately. The most common locations are the femoral neck and the spine.
Osteoporosis affects an estimated 6% of males and 22% of females over the age of 50 in Australia (2). These percentages only seem to increase as we get older, making it all the more important to maintain our bone health for as long as possible (2). Low BMD and osteoporosis have been linked with higher possibilities of fractures and bone breaks, longer healing times, greater joint pain, loss of muscle strength and a decrease in quality of life.
Risk Factors for Osteoporosis (3)
Many risk factors increase the risk of developing osteoporosis. Some of which are environmental/manageable, and others which you cannot change; such as being female and having a direct relative who experienced an osteoporotic fracture.

- A Lack of Physical Activity
- Low Vitamin D Levels
- Low Calcium Intake
- Tobacco Smoking
- Excessive Alcohol Consumption (>2 Standard drinks per day)
- Early Menopause (Before age 45)
- Long term use of medication such as Corticosteroids (check with GP)
Additionally, some chronic conditions may predispose you to become osteoporotic at a higher rate. Check with your GP if you have any of the following conditions to see if you have a higher risk of developing osteoporosis:
- Hyperthyroidism
- Rheumatoid arthritis
- Chronic liver/kidney disease
- Chronic Nutrient Absorption Conditions.
Diet and Exercise Recommendations
Diet recommendations (4)
A well-structured, varied diet is the backbone of maintaining good health; the same is said for maintaining strong and healthy bones. Calcium and Vitamin D are extremely important when it comes to bone health; therefore, it is recommended to ingest foods with high sources of Calcium and Vitamin D such as:

- Low-fat milk
- Low-fat yogurt
- Cheese
Vitamin D
- Salmon
- Tuna
- Mackerel
- Sardines
Additionally, bone strength can be improved through eating a variety of other vitamins and minerals such as Vitamin C & K, Magnesium and Potassium. You may check this list of foods that help maintain bone health.
It should also be noted that excessive drinking of alcohol (>2 Standard drinks per day) may lead to the increased loss of bone matter. In addition, excess caffeine intake (coffee/soda) may limit the amount of calcium absorbed by the body. It would be wise to monitor your consumption of both these factors to ensure optimum bone health.
Exercise Recommendations

3 forms of exercise can be utilised to help treat osteoporosis:
- Weight-Bearing Exercise
- Resistance Exercise
- Balance Training
Come and see us for a chronic disease management plan to help with your osteoporosis.
Weight-Bearing and Resistance Exercise Training

- Walking
- Impact Training
- Body Weight Exercises
- Weight Training
Other Forms of Aerobic Exercise
Balance Training

- Reaction Training
- Static Balance Training
- Dynamic Balance Training
- Proprioceptive Training
Exercises to Avoid (3-5)
As mentioned previously, all exercise should be provided and consulted with either an Exercise Physiologist to minimise the chance of injury and fracture, and to maximise the benefits of bone growth.
Those who are osteopenic and osteoporotic have the possibility of experiencing unexpected fractures/breaks while completing heavy lifting and/or high-intensity exercise. This far out weights the possible benefits of bone regrowth through this form of exercise. Therefore, get in touch with an allied health professional before partaking in physical activity aimed at improving your bone health.
Other Treatment Options (3-4, 6)
Other treatments/management methods of Osteoporosis include the use of medications and supplements to ensure the intake of the requires nutrients and minerals to keep our bones healthy.
Supplements are a great way of ingesting essential vitamins and minerals for bone health if we are unable to get these nutrients through our diet. These supplements include:
- Calcium
- Vitamin D, C & K
- Magnesium
- Potassium
If lifestyle interventions fail or are not beneficial for your specific medical history at improving bone health, another option includes the use of medications. Depending on your current health and medical history will determine which medication you will be placed on. Generally, the first line of medication used is Bisphosphonates to slow down bone degeneration.
Other medications that may be used to help treat osteoporosis include but are not limited to:
Sex Hormone Therapy (Estrogen – Women, Testosterone – Men)
- Other Hormone Therapy (Parathyroid Hormone)
- Receptor Modulating Therapy
- Denosumab injections (2x per year)
Do not solely rely on medication for osteoporosis prevention/management, it should be used in conjunction with lifestyle interventions with the guide of your GP and other allied health practitioners.
We Can Help
Here at Fortitude Exercise Physiology, we have a number of treatment pathways that can assist you in your pursuit to improved muscular and bone strength. Learn more about our services here. Alternatively, we would love to hear from you directly via our enquiry form below:
References
- Organization WH. WHO Technical Report Series: World Health Organization; 1994.
- Wade S, Strader C, Fitzpatrick L, Anthony M, O’Malley C. Estimating prevalence of osteoporosis: examples from industrialized countries. Archives of osteoporosis. 2014;9(1):1-10.
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/osteoporosis
- https://www.nof.org/patients/treatment/nutrition/
- Sinaki M. Osteoporosis. Braddom’s Physical Medicine and Rehabilitation: Elsevier; 2021. p. 690-714. e3.
- https://www.mayoclinic.org/diseases-conditions/osteoporosis/in-depth/osteoporosis-treatment/art-20046869 – For medications


 Sex Hormone Therapy (Estrogen – Women, Testosterone – Men)
Sex Hormone Therapy (Estrogen – Women, Testosterone – Men)

