What is PCOS?
PCOS, also known as polycystic ovarian syndrome is a condition that affects the ovaries, hormones and reproductive organs of the female reproductive system.
Common Signs/Symptoms to Look Out for (1,2)
It is important to understand the basics of PCOS so that you can identify any signs and/or symptoms of PCOS yourself. This will increase the chance of an early diagnosis of PCOS and early management/treatment options to help. Signs and symptoms of PCOS often begin developing around the time of the first menstrual period during puberty. Occasionally PCOS develops later in life, however, this is usually in response to a significant bout of weight gain.
PCOS signs and symptoms may vary from person to person, particularly with individually experienced intensity; however, a diagnosis of PCOS is often made when an individual experiences at least 2 of the following signs and/or symptoms:
- Irregular Periods: Infrequent, irregular, or prolonged menstrual cycles are the most common sign of PCOS. Examples may include extended periods between menstrual cycles (35+ days) and frequent abnormally heavy periods.
- Excess Androgen: Abnormally high levels of male hormones such as testosterone may result in various physical signs. A common occurrence is the expression of excess facial and body hair (hirsutism), and more rarely the expression of severe acne and male-pattern baldness.
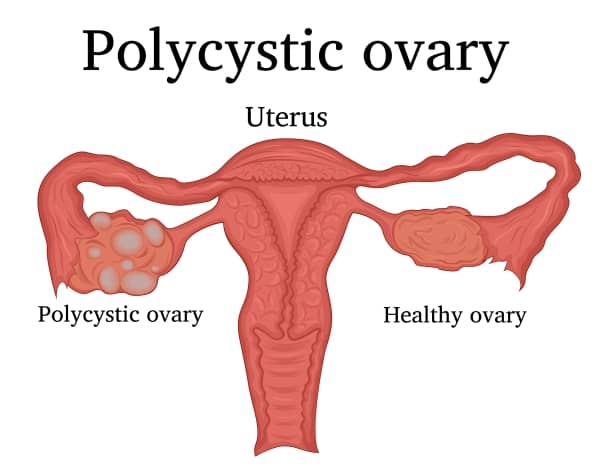
- Polycystic Ovaries: In some circumstances, your ovaries may become enlarged and swollen, containing follicles
surrounding the eggs. This results in the ovaries failing to function regularly (irregular/infrequent periods).
It may be best to seek a doctor or medical physician’s help if you are concerned and are experiencing some of the common signs and symptoms of PCOS (irregular periods, excess body and facial hair, severe acne, etc.).
Causes (1,2)
- Excess Insulin: Insulin is the primary hormone promoting the uptake of sugar into the body’s cells, this is the body’s primary energy supplier. A poor diet, exercise routine, and an increase in weight (particularly around the abdominal region) may begin a chain reaction that leads to insulin resistance. Insulin resistance results from the body blocking, or simply not being able to identify insulin and its ability to react with the body. This results in blood glucose levels rising, an excess amount of insulin secreted, and an increased amount of androgen produced, all of which lead to difficulties with ovulation and regular menstrual cycles.
- Hereditary: A vast amount of research suggests that genetics may play a role in the development of PCOS. If you know of family members that have insulin resistance and/or PCOS, it may be wise to book an appointment with your GP or medical practitioner to discuss your likelihood of having PCOS and what you can do to help mitigate the chance of developing PCOS yourself.
- Excess Androgen: The ovaries produce abnormally high levels of androgen, which results in hirsutism (growth of excess hair on the face and body) and acne.
Complications (1,2)
Many complications can arise from PCOS, some more severe than others. However, all should be acknowledged as possible complications.
Major complications include:
- Infertility
- Gestational diabetes and pregnancy-induced high blood pressure
- Miscarriage and premature birth
- Metabolic syndrome, type 2 diabetes and/or prediabetes
- NASH – A severe liver disease/inflammation caused by the
accumulation of fat in the liver.
Other complications may include:
- Sleep apnoea
- Depression
- Anxiety
- Eating disorders
- Obesity
Rarer complications include:
- Abnormal and intermittent uterine bleeding
- Cancer of the uterine lining (endometrial cancer)
Typical Treatments for PCOS
Your GP may give provide a versatile list of strategies to help manage your PCOS which are outlined below. Additionally, some strategies can be implemented if you are trying for pregnancy.
Medication (3)
Medication is a staple intervention to help manage PCOS. To help better regulate your menstrual cycle, your GP may recommend the use of medications such as:
- Birth Control Pills: These pills contain estrogen and progestin decrease androgen products that help to better regulate estrogen.
- Progestin Therapy: Taking progestin between 10-14 days every month or the second month can help better regulate your periods and perhaps protect against certain cancers.
- Metformin: An oral medication for those with Type 2 Diabetes to improve insulin resistance and lower insulin levels within the blood. This treatment can also help mitigate the possibility of developing type 2 diabetes in the future if you have pre-diabetes or have had gestational diabetes in the past.
Alternatively, your doctor or GP may prescribe the following medications to help with ovulation if you’re struggling with pregnancy:
- Clomiphene: The most common medication prescribed to help ovulation. This oral anti-estrogen medication is taken during the first part of your menstrual cycle.
- Letrozole (Femara): A breast cancer-specific treatment that can help stimulate the ovaries.
- Gonadotropins: Hormonal medications that are prescribed and delivered via injections.
Before beginning any medication treatment, you should always consult your GP or medical practitioner for their professional opinion on what works best for you. In addition to medicinal assistance, your GP will suggest implementing lifestyle interventions to help manage your PCOS from a holistic approach.
A combination of dietary recommendations and physical activity is generally the best course of action to manage PCOS as best as possible. Generally speaking, reducing weight and maintaining a healthy weight is a great way to help lower insulin levels and help regulate ovulation.
Diet (4)
A healthy diet is a staple intervention for managing PCOS. Broadly, minimising high carbohydrate foods such as white rice, pasta, and white bread is an effective option to manage PCOS. A high carbohydrate diet may lead to increased insulin levels. In general, low-carbohydrate diets have been shown to decrease insulin levels and regulate glucose levels within the body, minimising the likelihood of serious long-term complications and increasing fertility. General recommendations include minimising carbohydrates, increasing complex fats and maximising lean proteins.
Exercise (5)
Exercise is a great way to lower blood sugar levels and stabilise insulin resistance within the body. Some research even indicates that incorporating a regular exercise regime into your daily/weekly schedule may even treat and prevent insulin resistance. Although we know that it is a good idea to exercise to help manage PCOS, it can be quite overwhelming to determine what is the best form of exercise to complete, especially when there are so many forms and variations of exercise available. We at Fortitude Exercise Physiology can help you create a management plan to help you.
Optimising Exercise for PCOS
The best form of exercise to help manage PCOS is based on a multimodal approach. This involves an exercise program that incorporates both resistance (weight training) and aerobic (cardio) exercise. Ideally completing the resistance exercise component before your cardio, would ensure that you aren’t too fatigued while completing your resistance training, allowing for the greatest beneficial outcomes from your strength and conditioning.
The best form of resistance exercises to complete involves compound exercises. These exercises involve multiple muscles that attach across multiple different joints to lift the weight. Compound exercises will ensure that you’re getting the most bang for your buck when it comes to exercise. Completing resistance exercises will help build muscle within the body. Although this won’t bulk you up, it will be a great source of tissue to help boost your metabolism! The greater abundance of muscle within the body will assist with there being less insulin within the bloodstream. Not only this, the more muscle you have within your body, the greater boost your metabolism will receive, further assisting insulin and menstrual cycle control.
Simple Yet Effective Exercises
Outlined below are some simple yet effective at-home exercises to help manage your PCOS. Just remember to complete these before your walk for the best results!
Sit-to-Stands/Goblet Squats

Glute Bridges

Wall/Incline/Floor Push-ups

References:
- https://www.healthline.com/health/polycystic-ovary-disease#medical-treatments
- https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
- https://www.mayoclinic.org/diseases-conditions/pcos/diagnosis-treatment/drc-20353443
- https://www.healthline.com/health/pcos-diet
- https://exerciseright.com.au/best-types-exercise-pcos/#:~:text=CARDIO&text=Moderate%20exercise%20like%20brisk%20walking,disease%20and%20type%202%20diabetes.